Over the past 40 years, the rate of those suffering from cervical cancer has dropped by more than 50 percent due to the successful implementation of tests to diagnose precancerous cells, improved treatment and vaccination for the disease. Cervical cancer is no longer the most common cause of cancer-related deaths for women in Portland, but the disease continues to affect more than 14,000 women across the United States, annually. January, Cervical Health Awareness Month, recognized by the U.S. Congress, is a time when the National Cervical Cancer Coalition offers a range of resources to educate the public and healthcare providers about cervical health.
Doctors and nurses at The Portland Clinic are taking additional steps to help keep our neighbors informed this month, working to ensure the health and well-being of all women in the Portland area. With a strong roster of women’s health specialists and gynecologists, The Portland Clinic encourages women to begin screening for cervical cancer at the age of 21.
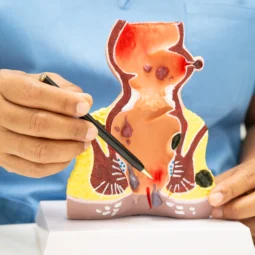
There are two main types of cervical cancer:
Squamous cell carcinoma is the more common of the two types, accounting for 80 to 90 percent of cervical cancer cases. In this circumstance, the cancerous cells start in the lining at the bottom of the cervix — the narrow end of a woman’s uterus, located at the top of the vagina.
In cases of adenocarcinoma, which is diagnosed in about 10 to 20 percent of patients, the cancer cells are located in the upper portion of the cervix.
There are cases of patients suffering from both types of cervical cancers. Occasionally, metastatic cervical cancer occurs, which is the spreading of squamous cell carcinomas and/or adenocarcinomas outside the cervix, throughout the body.
Human papillomavirus (HPV) is a family of more than 200 viruses, all of which are spread by sexual activity. HPV is highly present in the diagnosis of cervical cancer. In fact, nearly 70 percent of patients who develop cervical cancer have HPV. More than 14 million new infections of HPV occur each year in the U.S. Three vaccinations are available to prevent HPV, but they will not treat the virus if already contracted.
The Center for Disease Control and Prevention recommends females receive the HPV vaccines before they become sexually active and exposed to HPV. Eleven and 12 are the recommended ages, but females aged 13 to 26 who have not received the vaccinations or completed the series may still receive them. Sexually active women who have not received the vaccinations may still receive the injections, but may have been exposed to types of HPV that would have been prevented by the vaccine.
Most women with early stage cervical cancer do not have symptoms. Some women may experience:
- Vaginal bleeding: This includes bleeding between periods, after sexual intercourse or postmenopausal bleeding.
- Unusual vaginal discharge: A watery, pink or foul-smelling discharge is common.
- Pelvic pain: Pain during intercourse or at other times may be a sign of abnormal changes to the cervix, or less serious conditions.
All of these cervical cancer symptoms should be discussed with your gynecologist.
Signs of advanced stages of cervical cancer:
- Weight loss
- Fatigue
- Back pain
- Leg pain or swelling
- Leakage of urine or feces from the vagina
- Bone fractures
How do we fight cervical cancer?
Prevention and early detection are the best options in fighting the disease. The Papanicolau (Pap) test — or Pap smear — involves a physician collecting cells directly from the cervix. It’s a short procedure to help physicians look for unusual changes in the cells of the cervix, which may lead to cancer in the future. It is imperative to diagnose any abnormal changes to minimize the spreading of cancerous cells.
Treatments:
There are multiple treatment scenarios for abnormal cervical cells, each weighing on multiple aspects of reproductive health, including whether a woman chooses to attack the disease with the ambition to remain fertile.
Treatment options may include:
- Cryosurgery
- Laser surgery
- Loop electrosurgical excision procedure
- Cold knife conization
- Simple hysterectomy (as the first treatment or if the cancer returns after other treatments)
Treatment options for adenocarcinoma in situ include:
- Hysterectomy
- Cone biopsy (a possible option for women who wish to have children)
If you have any questions or concerns regarding HPV or cervical cancer, doctors and nurses at The Portland Clinic are available by appointment to provide you with an exam or information on prevention, diagnosis and treatment. Appointments can be scheduled by calling 503-223-3113 or by booking online.
You can join in on the conversation on Twitter, following and contributing to the hashtag #CervicalHealthMonth.